
Understanding Shoulder Pain: Atraumatic and Traumatic Shoulder Instability
Shoulder pain is a common complaint among people of all ages. It can be caused by various factors, but two often seen causes are atraumatic and traumatic shoulder instability. These conditions can lead to further shoulder injury and pain when moving the arm overhead or behind the back. In this blog post, we’ll delve into what these conditions are, their risk factors, symptoms, and how physiotherapy can help manage them.
Atraumatic Shoulder Instability: What is it?
The shoulder is a complex joint, and its stability is crucial for our daily activities. Atraumatic Multidirectional Instability (MDI) is a condition where the shoulder joint becomes unstable in multiple directions due to an individual’s physiology which contributes to instability. This instability can manifest in four types: loose shoulder, voluntary dislocation, habitual dislocation, and sustained subluxation.
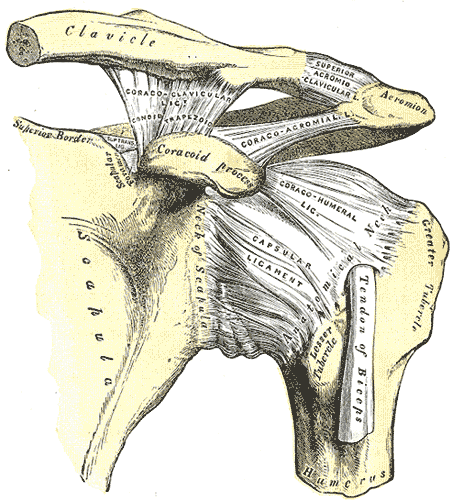
Shoulder Joint, Henry Vandyke Carter, Public domain, via Wikimedia Commons
Risk Factors and Causes
Atraumatic MDI is commonly seen in athletes who frequently perform overhead movements such as gymnasts, swimmers, and weightlifters. These activities can lead to repetitive microtrauma of tissues around the shoulder, contributing to shoulder instability. However, it’s important to note that ligament laxity alone is not the only determinant in the development of atraumatic MDI. Other factors such as weak dynamic stabilizers, neuromuscular disturbances, congenital bony abnormalities, redundant capsules, hypoplastic labrums, and disturbances in collagen production can also predispose an individual to shoulder instability.
Symptoms
People with atraumatic MDI often experience a mild generalized ache around the shoulder, a sensation of instability when lifting objects, and a heavy sensation within the shoulder girdle. Other characteristics of instability, such as general ligament laxity, bilateral shoulder laxity, or a family history of similar conditions, are typically found in patients diagnosed with Atraumatic MDI.
Traumatic Shoulder Instability: What is it?
Traumatic shoulder instability (TSI) occurs when a force, such as a fall on an outstretched hand (FOOSH) or an external force that places the arm in excessive abduction and external rotation, causes a dislocation or subluxation of the shoulder joint. This injury can damage one or more of the supporting structures, leading to shoulder instability.
Traumatic shoulder instability is more common among young and active individuals, especially those under the age of 30. Nearly half of all shoulder dislocations occur in patients aged 15 to 29 years old, with the highest rate of recurrent dislocations found in those under age 30, more often males. Understanding the optimal management of traumatic anterior shoulder dislocations is crucial for long-term benefits, as recurrent shoulder instability usually develops within the first 2 years of primary dislocation.
Risk Factors and Causes
TSI can be caused by various incidents, but a common cause is a fall on an outstretched hand or an external force that places the arm in excessive abduction and external rotation. Anterior shoulder dislocations are most common, followed by posterior or inferior dislocations.
Symptoms
Acute symptoms of TSI may include pain, a painful reduction in range of motion, swelling, and visible dislocation. Individuals may also experience symptoms when in a position of instability, such as pain, apprehension, guarding, slipping, popping, subluxation, or dislocation.
Associated Complications
Complications associated with shoulder dislocations can include nerve and vascular involvement. These complications require prompt attention and can be confirmed with additional imaging if suspected on physical examination. Labral and rotator cuff tears can be a secondary injury to a traumatic dislocation.
Physiotherapy Treatment Approach
At Connect Physiotherapy & Exercise in Edmonton, we believe in a comprehensive approach to managing shoulder instability. Treatment for both atraumatic and traumatic shoulder instability typically involves non-operative rehabilitation, with surgical intervention only considered if conservative management fails. Our physiotherapy treatment approach focuses on restoring range of motion (ROM), strengthening of scapular and humeral head stabilizers, and improving neuromuscular control of the shoulder complex. We also incorporate manual therapy based on the direction of instability.
Exercise Examples
Our physiotherapists may recommend exercises such as protraction/retraction strengthening exercises, eccentric strengthening of internal and external rotation at the shoulder, and wall stabilization drills. These exercises aim to improve shoulder stability and reduce shoulder pain.
Manual Therapy
Manual therapy for shoulder instability is largely based on the direction of instability. For anterior instability, mobilization techniques of the glenohumeral joint are acceptable in all directions except for anteriorly. For issues that pertain to extracapsular tissues, massage and stretching may be useful.
Management and Prognosis
The management of shoulder dislocations involves timely reduction and immobilization. Surgical treatment may be considered for patients under 30, non-surgical treatment has been associated with significantly higher rates of recurrent dislocation outside of young adolescents. The decision to return to sport should be based on symmetric range of motion and strength in comparison to the healthy shoulder, as well as in consultation with a physician.
Shoulder instability, whether atraumatic or traumatic, can significantly impact your daily life and activities. However, with the right physiotherapy treatment approach, it’s possible to manage these conditions effectively and reduce shoulder pain. At Connect Physiotherapy & Exercise, we’re committed to helping you regain your shoulder stability and improve your quality of life. If you’re experiencing shoulder instability or shoulder pain, don’t hesitate to book an appointment with us today.
*Remember, while knowledge is power, self-diagnosis and treatment can be risky. While this blog provides useful information, it’s essential to see a trained professional for proper diagnosis and management. Every person is unique, and so is their recovery journey. At Connect Physiotherapy & Exercise, we’re all about personalized care. Let us help you navigate your path to recovery
References:
An, Y. H., & Friedman, R. J. (2000). Multidirectional instability of the glenohumeral joint. Orthopedic Clinics of North America, 31(2), 275-283.
Cordasco, F. A. (2000). Understanding Multidirectional Instability of the Shoulder. Journal of Athletic Training, 35(3), 278-285.
Itoi, E. (2004). Pathophysiology and Treatment of Atraumatic Instability of the Shoulder. Journal of Orthopaedic Science, 9: 208-213.
Kuroda, S., Sumiyoshi, T., Moriishi, J., Maruta, K., and Ishige, Noriyuki. (2001). The Natural Course of Atraumatic Shoulder Instability. Journal of Shoulder and Elbow Surgery, 10(2): 100-104.
Wilk, K. E., Macrina, L. C., and Reinold, M. M. (2006). Non-Operative Rehabilitation for Traumatic and Atraumatic Glenohumeral Instability. North American Journal of Sports Physical Therapy, 1(1)
Hasebroock AW, Brinkman J, Foster L, Bowens JP. Management of primary anterior shoulder dislocations: a narrative review. Sports Med Open. 2019 Jul 11;5(1):31
Photo accessed at: https://commons.wikimedia.org/wiki/File:Gray326.png

