
Understanding Patellofemoral Pain Syndome
Welcome to our guide on Patellofemoral Pain Syndrome (PFPS), commonly known as runner’s knee. If you’re experiencing knee pain during activities like walking, running, or even using stairs, you’re not alone. PFPS, characterized by an ache in the front of your knee, is the leading cause of knee pain in the active population. With a prevalence of 12-15% in the overall population, and women being twice as likely to develop it, PFPS is a condition that affects many. This guide will help you understand the anatomy of your knee, the role of the patellofemoral joint, and how imbalances can lead to pain. We’re here to provide practical information to manage this common knee injury effectively.
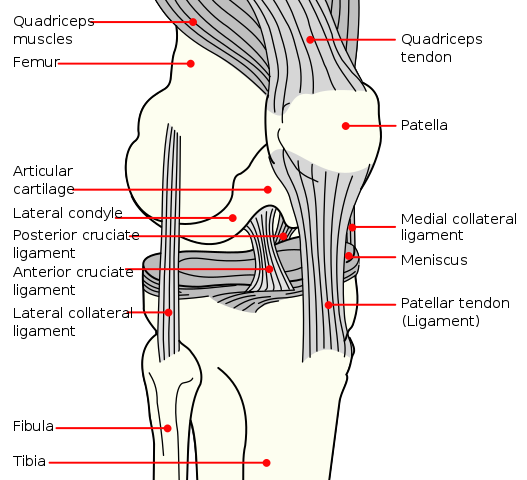
The Anatomy of Your Knee and Causes of PFPS
Your knee joint is composed of three bones: the femur (thigh bone), the tibia (shin bone), and the patella (kneecap). The patella, or kneecap, plays a pivotal role in knee movement, especially during activities like walking, running, and jumping. However, these movements subject the patella to substantial load and forces. For instance, the patellofemoral joint experiences forces up to 1.3x body weight during walking, 3.3x during stair climbing, and a staggering 7.8x during deep knee bends. The degree of knee bend during an activity significantly influences the compressive force experienced at the knee joint.
The patellofemoral joint is where the patella interacts with the femur, ensuring smooth knee movement and stability. This joint facilitates the harmonious glide of your patella in the femoral groove during your daily activities. However, imbalances, misalignments, or structural issues can disrupt this smooth operation, leading to PFPS and discomfort.
While the exact cause of PFPS remains unclear, potential triggers include overuse, overloading, and improper alignment of the patellofemoral joint. Rarely is there only one factor contributing to this condition. Predisposing factors that increase stress on the patellofemoral joint fall into three main categories:
– Bony abnormalities such as a shallow trochlear groove or poor articulation of the femoral and patellar surfaces.
– Lower extremity malalignment, including flat feet or foot pronation, and an increased Q angle in women.
– Soft tissue imbalances, such as tight lateral structures (IT band or Vastus Lateralis), weak medial structures (Vastus Medialis Obliquus [VMO]), ligament laxity, and weak hip muscles.
It’s worth noting that PFPS can also cause discomfort in other areas around the knee joint.
 Mysid, Public domain, via Wikimedia Commons
Mysid, Public domain, via Wikimedia Commons
The Role of Physiotherapy in Managing PFPS
Physiotherapy can play an important role in managing PFPS. Most people are able to manage PFPS conservatively, with activity modification and exercise. A study found that symptoms improved naturally if no obvious biomechanical malalignment was present. The conservative treatment includes symptom control through methods like ice, NSAIDS, patellar taping/bracing, and neoprene sleeves. Identifying specific triggers and avoiding activities that exacerbate the pain is also part of the treatment approach.
Therapeutic exercises are designed to correct imbalances of the entire kinetic chain. This includes stretching, strengthening, proprioception, and recruitment exercises. Examples of these exercises include closed chain quadriceps strengthening exercises with proper alignment such as lunges, squats, and leg press. Specific VMO strengthening/recruitment exercises like lateral step-ups with a block, straight leg raise, and terminal knee extension have also shown benefit. Stretching of lateral structures that tend to be tight, like the IT band and Vastus Lateralis, is also recommended.
Manual therapy is another component of the conservative treatment approach. For patients presenting with abnormal patellar glides, patellar mobility techniques may be employed, taking care not to compress the joint. Techniques such as myofascial release, soft tissue mobilization, and massage therapy involving the muscles and soft tissue of the legs and hips have been shown to be effective in reducing symptoms. Stretching of the IT band, hamstrings, and other tight structures is an important component of manual therapy. Proprioceptive neuromuscular facilitation (PNF), based on the principles of autogenic and reciprocal inhibition, increases muscle strength, recruitment, and flexibility.
Working with a Rehabilitation Professional
To address PFPS effectively, it’s important to work with a trusted rehabilitation professional, such as a physiotherapist. They will guide you through a comprehensive assessment to understand your specific situation and create a personalized treatment plan. This plan will include a tailored exercise regimen aimed at strengthening the hip, thigh, and knee muscles, improving joint stability, promoting proper movement patterns, and addressing muscle imbalances. They can also advise on activities to include and/or avoid to not exacerbate symptoms.
Your physiotherapist may also use manual therapy techniques to alleviate pain, improve joint mobility, and enhance tissue function. They will assess your movement patterns to identify any biomechanical issues contributing to your PFPS and provide guidance on correcting these patterns. Pain management strategies such as taping, bracing, or orthotics may be suggested to provide temporary relief and support during activities.
Each person’s management of PFPS is unique, Embrace the guidance of your rehabilitation professional and stay committed to your treatment plan. With their support and your dedication, you can effectively manage PFPS and improve your knee health. If you have any further questions or need additional guidance, our dedicated team at Connect Physiotherapy & Exercise in Edmonton is here to support you on your path to healthy knees.
*Remember, while knowledge is power, self-diagnosis and treatment can be risky. While this blog provides useful information, it’s essential to see a trained professional for proper diagnosis and management. Every person is unique, and so is their recovery journey. At Connect Physiotherapy & Exercise, we’re all about personalized care. Let us help you navigate your path to recovery
References
Neumann, D. A. (2016). Kinesiology of the musculoskeletal system (3rd ed.). Mosby.
Boling, M., Padua, D., Marshall, S., Guskiewicz, K., Pyne, S., & Beutler, A. (2010). Gender differences in the incidence and prevalence of patellofemoral pain syndrome. Scandinavian Journal of Medicine and Science in Sports, 20(5), 725- 730
Reid, R. C. (1992). Anterior knee pain and the patellofemoral pain syndrome. In L. Burgess, & D. Terry (Eds.), Sports injury assessment and rehabilitation (pp. 345-398). New York, NY: Churchill Livingstone Inc.
Collado, H., & Fredericson, M. (2010). Patellofemoral pain syndrome. Clinics in Sports Medicine, 29(3), 379-398.
American Academy of Health and Fitness Professionals. (1996). Patello-femoral syndrome post rehab protocol. Sacramento, CA: Author.

